Cardiovascular diseases (CVD) are the leading cause of mortality in the Philippines. Hypertension is the most important risk factor for CVD. Despite advancements in hypertension medications, blood pressure (BP) control remains suboptimal. In order to improve the management of hypertension we propose a lifestyle intervention delivered through SMS (Short Messaging Service). Given its widespread use in the Philippines and Vietnam, SMS is an accessible, cost-effective method to engage patients and their family members in the management of hypertension. The MESSAGE US (Managing blood prESSure by AddinG tEchnology and Using Social support) Study is a 6-month, assessor-blinded, 3-arm RCT to examine whether hypertension education, delivered through SMS messages to patients and their family members, will lead to improved BP outcomes. Building on previous mobile health interventions, we have designed a combined intervention that capitalizes on the previously reported health-promoting effect of social support networks. Participants will be allocated in 1:1:1 ratio to either control (participants receive weekly reminders to check their BP), individual-only SMS (participants receive weekly reminders to check their BP and information on hypertension), or social support SMS (the participant receives reminders to check BP and hypertension information and 1 family member receives social support prompts). We hypothesize that the individual-only SMS arm will show improved BP control over the control arm, and that the social support SMS arm will have better BP control than both the other arms of the trial.
Co-Principal Investigators:
Julieta Gabiola, MD, FACP
Clinical Professor of Medicine
Educators for CARE faculty
CIGH Faculty Fellow
Stanford University
(650) 736-5211
Bui The Dung, MD, PhD
Department of Cardiology University Medical Center, HCM city
Arthur Gallo, MD
Chief Medical Officer
ABC’s for Global Health Foundation Inc.
Students:
Joyce Macalalad
University of California, Los Angeles
Whitney Chan
University of California, Los Angeles
Lauren Tran University of California, Los Angeles
Latha Palaniappan, MD, MS
Clinical Professor
Division of Primary Care and Population Health
Stanford University School of Medicine
(650) 498-9325
Dang Nguyen, BS
Department of Cardiology
University Medical Center, HCM city
(713) 505-7713
On-site Collaborators:
- University of the Assumption, Pampanga
- Holy Angel University, Pampanga
- Angeles University Foundation, Pampanga
- Barangay Health Workers in 20 Barangays in Pampanga
- SACOP Social Action Center of Pampanga
Other Staff:
Melinda Bender
Ma. Hilana Roman (statistician)
Jethro M. Ocampo, RPh
Carolina D. Manansala-Yap
Michael B. Quiambao Ariagna
INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of death globally, with nearly three quarters of these deaths occurring in low and middle income countries (LMIC) (1). Hypertension is the primary modifiable risk factor for CVD (2) and the greatest risk factor for morbidity and mortality worldwide (3). This global disease burden is reflected in the Philippines, where hypertension affects 1 in 4 and ischemic heart disease and stroke are the top two causes of mortality (4, 5).
Despite pharmacologic advancements in the treatment of hypertension, the percentage of known hypertensives with controlled blood pressure (BP) remains alarmingly low in LMICs (6). While strong patient engagement and constant surveillance are cornerstones of successful chronic disease management (7), they are difficult to achieve when nearly half of Filipinos live on less than $2.00 a day and cannot afford regular care (8). Without continuity of care, low-income individuals are particularly vulnerable to progressive complications from uncontrolled hypertension. In the setting of insufficient health resources and high out-of-pocket expenditures, we need a low-cost, efficient, and widely accessible medium for physicians to provide health education and continuity of care to chronic disease patients.
Short Messaging Service (SMS) is one promising tool that has shown great success in increasing treatment adherence, symptom surveillance, appointment attendance and patient satisfaction in previous studies (9–13). While SMS has been studied in the management of chronic CVD, these studies have primarily been undertaken in high-income countries and had varying effectiveness (4)(15)(16).
an EMR system that is capable of sending automated SMS and tracking patient-reported BP readings[1] . The MESSAGE US Study offers development opportunities for students from multiple institutions, at varying stages of training. Dr. Julieta Gabiola and Dr. Latha Palaniappan will lead a team of students (from Stanford University School of Medicine, UC Davis Undergraduate Studies, and Nursing Colleges at the University of Assumption, Holy Angel University, and Angeles University Foundation[2] ) on study design and implementation. Nursing students will also develop clinical skills on health counseling and chronic disease management.[3]
SPECIFIC AIMS
The overall goal of the MESSAGE US Study is to demonstrate the efficacy of a text messaging intervention in disseminating health information and improving BP management in hypertensive patients. Our specific aims are as follows:
1) Determine whether informational SMS messages, targeted toward hypertensive patients in xxx, can lead to improved BP outcome.
2) Determine whether motivating social support, by sending SMS messages to patients’ family members, can lead to further reductions in BP.
3) Identify the benefits and limitations of using SMS to deliver health education. These limitations will guide the design of future studies, act as a model for SMS-based health interventions, and inform efforts to further optimize patient care
We will perform a six-month, assessor-blinded, three-arm randomized control trial to study whether informational text messages, sent to individual subjects and their family members, will lead to improved control of BP. 300 participants will be recruited from the medical mobile clinic, which currently serves 20 barangays(districts). Lifestyle intervention messages will be developed in collaboration with nursing faculty and students at three academic institutions in the Philippines and tested in a group of volunteers . A focus group will be formed to provide feedback on the content of these messages. Examples of lifestyle intervention messages include reminders to exercise, increase fruit and vegetable intake, and reduce sodium intake.
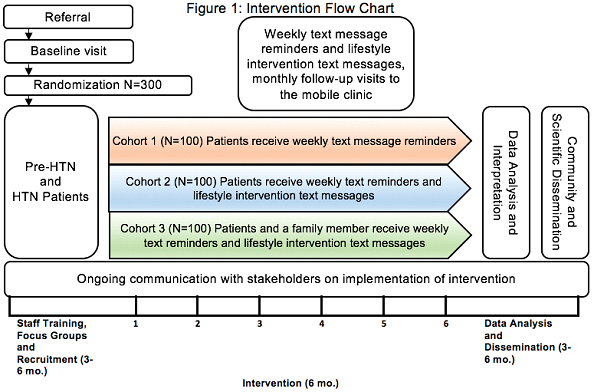
Enrolled patients will be allocated by computer-generated randomization in 1:1:1 ratio to either of three groups:
1. Control group: weekly BP check reminders
2. Individual intervention group: arm 1 (control) + weekly lifestyle messages
Content of the text sending Diet?
What is reminder means?
Include “weekly lifestyle message” content of the text sending
Diet?
3. Social support intervention group: arm 2 (individual intervention) + weekly lifestyle messages to supporter
The primary outcome will be change in BP, measured monthly over a period of six months. Secondary outcomes will include BMI, waist to hip ratio, hypertension knowledge, Hemoglobin A1c, patient perception of social support and self-efficacy, and adherence to medication, diet, and exercise prescriptions.
Inclusion/Exclusion: Patients will be eligible if they are over 18 years old; independently own and use their cellphone regularly; have a previous diagnosis of pre-hypertension or hypertension (130-159/80-99), or have had three consecutive visits with elevated systolic or diastolic BP; and have a family member (over 18 years old) with whom they can share their hypertension diagnosis. The family member must own and regularly use their own cell phone. No history of coronary artery disease, stroke, kidney disease and diabetes.
Sample size justification: We have excellent power (>99%) with a final sample size of 90/arm (100/arm recruited to allow for ~10% dropout) to detect a difference between the intervention and no text arms if we assume an average reduction as small as 3.6 mmHg over 6 months in the intervention groups compared to no change in the control group. Our assumptions about variance in SBP measures and within subject correlations are based on an earlier interventional study in nearby barangays.
Given the excellent power to detect an effect for the primary aim, we selected a sample size with sufficient power to address the secondary research question of whether the reduction differs in the social support vs individual arms. With 100/arm recruited, a final sample size of 90/arm, and assumed 6 month reductions of 10 mmHg in the social support arm and 7 mmHg in the individual arm, we will have 90% power.
Statistical methods : Analysis of variance for independent groups and Chi-square test
Linear mixed effects (LME) models will be fit to estimate the change in BP over time within each intervention group. We will include statistical interaction terms to allow us to test whether the intervention reduces BP over time (Aim 1) and whether the reduction differs between the two interventions (Aim 2). Both tests will be two-sided and performed at the 0.05 significance level. While we have plans in place to minimize missing data, we recognize that some data will be missing and any missing data will be fully described. LME models allow us to account for correlation between measures on the same subject while making flexible assumptions to appropriately account for any missing data. The intervention will be considered successful if we find the reduction in Aim 1 to be statistically significant.
TRANSFORMATIVE IMPACT
Individual impact: Given the strong, modifiable association between BP and CVD, even small reductions in BP can greatly improve quality of life and long-term survival in hypertensive patients. One meta-analysis found that an increase in BP by 20 mm Hg SBP or 10 mm Hg DBP doubled the observed rate of cardiovascular-related deaths in patients 40-69 years old (21).
Local impact: The results of the MESSAGE US Study will be used to guide SMS-based education and counseling programs at the ABC’s for Global Health Mobile Clinic, which is poised to serve about 40,000 people in Pampanga Province. MESSAGE US also draws on other local stakeholders including barangay health workers and three academic institutions. If this proof-of-concept is successful, it may lead to adoption and further development of the SMS-EMR platform by these stakeholders and other private and public sector care providers.
National impact: Filipinos send more SMS than any other nationality and account for 10% of the global volume of messages. Thus, a SMS-based health intervention may be more efficacious in the Philippines than in any other previously studied nation.
Contribution to the academic literature: If a 160-character SMS is to be used as a clinical tool to supplement physician-patient interactions, it must be guided by an understanding of behavior change and knowledge of the patient’s social resources (11, 14, 17, 22). Otherwise, SMS risks becoming a simple reminder tool, rather than a scalable platform to educate and motivate healthy lifestyles. To the best of our knowledge, we are the first study to examine whether SMS can be used to bolster patients’ social support systems, with measurable effects on BP.
LITERATURE
1. WHO | Cardiovascular diseases (CVDs) (2016) (available at http://www.who.int/mediacentre/factsheets/fs317/en/).
2. C. M. M. Lawes, S. Vander Hoorn, A. Rodgers, International Society of Hypertension, Global burden of blood-pressure-related disease, 2001. Lancet. 371, 1513–1518 (2008).
3. S. S. Lim et al., A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 380, 2224–2260 (2012).
4. World Health Organization, Philippines: WHO Statistical Profile, (available at http://www.who.int/gho/countries/phl.pdf).
5. R. G. Sy et al., Prevalence of atherosclerosis-related risk factors and diseases in the Philippines. J. Epidemiol. 22, 440–447 (2012).
6. M. Pereira, N. Lunet, A. Azevedo, H. Barros, Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J. Hypertens. 27, 963–975 (2009).
7. H. Holman, K. Lorig, Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 119, 239–243 (2004).
8. Website, (available at http://www.who.int/countryfocus/cooperation_strategy/ccsbrief_phl_en.pdf.).
9. S. Berrouiguet, E. Baca-García, S. Brandt, M. Walter, P. Courtet, Fundamentals for Future Mobile-Health (mHealth): A Systematic Review of Mobile Phone and Web-Based Text Messaging in Mental Health. J. Med. Internet Res. 18, e135 (2016).
10. T. de Jongh, G.-U. Ipek, V.-J. Vlasta, C. Josip, A. Rifat, in Reviews (2012).
11. T. A. Gurman, S. E. Rubin, A. A. Roess, Effectiveness of mHealth behavior change communication interventions in developing countries: a systematic review of the literature. J. Health Commun. 17 Suppl 1, 82–104 (2012).
12. R. T. Lester et al., Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 376, 1838–1845 (2010).
13. B. R. Devi et al., mHealth: An updated systematic review with a focus on HIV/AIDS and tuberculosis long term management using mobile phones. Comput. Methods Programs Biomed. 122, 257–265 (2015).
14. J. D. Piette et al., Mobile Health Devices as Tools for Worldwide Cardiovascular Risk Reduction and Disease Management. Circulation. 132, 2012–2027 (2015).
15. K. Bobrow et al., Mobile Phone Text Messages to Support Treatment Adherence in Adults With High Blood Pressure (SMS-Text Adherence Support [StAR]): A Single-Blind, Randomized Trial. Circulation. 133, 592–600 (2016).
16. J. C. Lauffenburger, N. K. Choudhry, Text Messaging and Patient Engagement in an Increasingly Mobile World. Circulation, CIRCULATIONAHA.116.021182 (2016).
17. C. Déglise, L. Suzanne Suggs, P. Odermatt, Short Message Service (SMS) Applications for Disease Prevention in Developing Countries. J. Med. Internet Res. 14 (2012), doi:10.2196/jmir.1823.
18. I. S. Harvey, K. Alexander, Perceived social support and preventive health behavioral outcomes among older women. J. Cross. Cult. Gerontol. 27, 275–290 (2012).
19. M. K. Campbell et al., The North Carolina Black Churches United for Better Health Project: intervention and process evaluation. Health Educ. Behav. 27, 241–253 (2000).
20. B. E. Ainsworth, S. Wilcox, W. W. Thompson, D. L. Richter, K. A. Henderson, Personal, social, and physical environmental correlates of physical activity in African-American women in South Carolina. Am. J. Prev. Med. 25, 23–29 (2003).
21. S. Lewington et al., Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 360, 1903–1913 (2002).
22. R. Whittaker, W. Robyn, M. Sally, D. Enid, M. Ralph, A Development and Evaluation Process for mHealth Interventions: Examples From New Zealand. J. Health Commun. 17, 11–21 (2012).
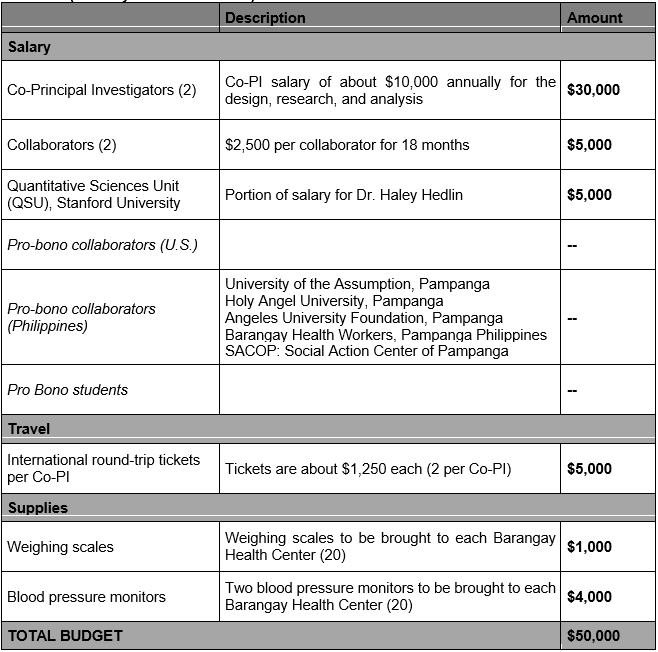
BUDGET (January 2017 – June 2018)